
Lymphoedema management:
The recommended management of lymphoedema in areas where lymphatic filariasis is endemic involves simple activities that have demonstrated their effectiveness in significantly improving the quality of life of patients. These activities include providing early detection of lymphoedema, caring for the skin by washing and drying the affected limb or area, preventing and treating entry lesions and providing lymph drainage by elevating the limb and exercising. These are the minimum activities that need to be undertaken, and there is a standard care beyond this that can be accessed where available.
Since the prevention and management of disability caused by lymphatic filariasis is now viewed as public health issue, the guidelines for the first level care worker developed by WHO to manage acute dermato-lymphangioadenitis (ADLA) are as follows:
TREATMENT FOR UNCOMPLICATED ADLA:
- Give analgesic such as paracetamol
- Give oral antibiotic such as amoxicillin for at least 8 days. In case of allergy to penicillin, oral erythromycin can be used;
- Clean the limb with antiseptic;
- Check for any wounds, cuts, abscesses and interdigital infection (especially between the toes). Clean with antiseptic, if any present. If local superficial skin infection is found give antibiotic cream, apply antifungal cream if interdigital infection is present;
- Give advice about prevention of chronic lymphoedema caused by lymphatic filariasis;
- Do not give antifilarial medicine.
- Home management includes drinking plenty of water, rest, elevation of the limb, wriggling the toes, cooling the limb with cold water and washing the limb if the patient can do it;
- Follow-up after 2 days at home. If situation does not improve, then refer the patient to physician.
MANAGEMENT OF SEVERE ADLA:

- Refer the patient to physician immediately to receive recommended antibiotic treatment
- Intravenous benzylpenicillin 5 million units given 3 times a day or intramuscular procain benzylpenicillin 5 million units given 2 times/day until fever subsides, then give oral phenoxymethylpenicillin 3 times/day. The minimum total treatment is atleast for 8 days.
- In case of allergy to penicillin give IV erythromycin lg 3 times/day until fever subsides, then give oral erythromycin lg given 3 times/day or give other antibiotic according to local situation.
- Give analgesic I antipyretic such as paracetamol
- Do not give any antifilarial medicine.
FILARIA SURVEY:
The size of the sample to be examined in a filaria survey varies with the type of survey, whether it is a routine survey or survey for evaluation. A filaria survey comprises the following elements:
MASS BLOOD SURVEY:
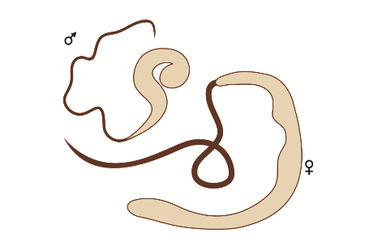
The definitive diagnosis of lymphatic filariasis depends upon the demonstration of living parasites in the human body. This calls for a night blood survey.
The thick film:
The thick film made from capillary blood is still the most commonly used method for epidemiological assessment. 20 cu. mm of blood is collected by a deep finger prick between 8.30 pm and 12 mid-night.
Membrane filter concentration (MFC) methods:
The most sensitive method currently available for detecting low density micro-filaraemia in the blood is by concentration techniques.
DEC provocation test:
Mf can be induced to appear in blood in the daytime by administering diethylcarbamazine (DEC) 100 mg orally.
CLINICAL SURVEY:
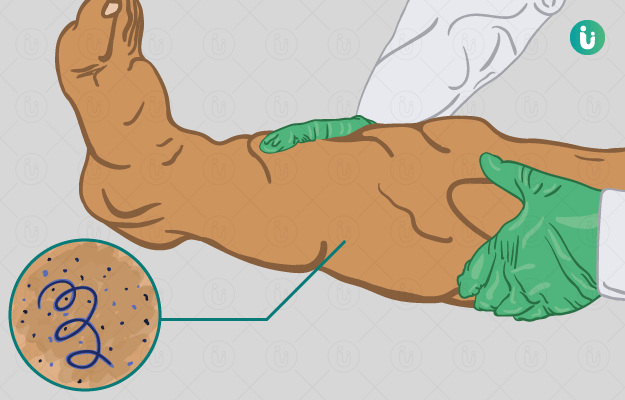
At the same time when blood is collected,. the people are examined for clinical manifestations of filariasis which should be recorded in the suggested schedule.
SEROLOGICAL TESTS:
Serological tests to detect antibodies to Mf and adults using immunofluorescent and complement-fixing techniques cannot distinguish between past and present infection, and heavy and light parasite loads in the human hosts.
XENODIAGNOSIS:
The mosquitoes are allowed to feed on the patient, and then dissected 2 weeks later. Where other techniques may fail, this may succeed in detecting low-density microfilaraemia.
ENTOMOLOGICAL SURVEY:
This comprises of general mosquito collection from houses, dissection of female vector species for detection of developmental forms of the parasite, a study of the extent and type of breeding places and other bionomics of mosquitoes.
CONTROL MEASURES:
The current strategy of filariasis control is based on :
- chemotherapy
- vector control
Chemotherapy:
Diethylcarbamazine:
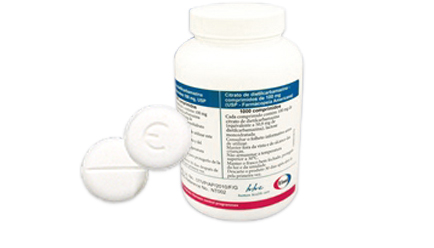
Diethylcarbamazine {DEC) is both safe and effective. The dose of DEC that is most generally accepted for the
treatment of Bancroftian filariasis is 6 mg/kg body weight per day orally for 12 days, given preferably in divided doses after meals. This amounts to a total of 72 mg of DEC per kg of body weight as a full treatment. For Brugian filariasis, recommended doses range from 3 to 6 mg of DEC/kg body weight per day, up to a total dose of 36-72 mg DEC/kg body weight as a full treatment.
DEC is rapidly absorbed after oral administration, reaching peak blood levels in 1-2 hours. It is also rapidly, excreted the blood half-life is only 2-3 hours in alkaline urine and about 10-20 hours in acid urine. DEC is given only to those who are Mf positive. It is generally accepted that selective treatment may be more
suitable in areas of low endemicity than in highly endemic, areas.
Ivermectin:
Ivermectin is a semisynthetic macrolide antibiotic with a broad spectrum of activity against a variety of nematodes and ectoparasites. The dose is 150-200 μg/kg of body weight. Ivermectin is not used in India. It is used in the region of Africa. There is no drug toxicity in normal persons. However, in microfilaraemic patients there may be a variety of reactions as a result of inflammatory response triggered by the cleared and dying microfilariae.
Vector control:
Where mass treatment with DEC is impracticable, the control of filariasis must depend upon vector control. Vector control may also be beneficial when used in conjunction with mass treatment.
Antilarval measures:
The ideal method of vector control would be elimination of breeding places by providing adequate sanitation and underground waste-water disposal system. This involves considerable expenditure amounting to several crores of rupees. Because of financial constraints, this may not be feasible in developing countries such as India in the near future. For the time being, therefore, vector control must be based on temporary or recurrent methods.
The current approach in India is to restrict the antilarval measures to urban areas, because it is operationally difficult and very costly to cover the vast rural areas of the country. The urban areas include an extra 3-km peripheral belt because the flight range of Culex quinquefasciatus (C. fatigans) is about 3 km.
(a) Mosquito larvicidal oil: Mosquito larvicidal oil (MLO) is active against all preadult
stages. It has. been the main chemical used to control C. quinquefasciatus for some time. Since it has proved to be less efficient under field conditions and more expensive than other chemical preparations, it is being replaced by pyrethrum oil, temephos and fenthion. (b) Pyrosene oil- E : This is a pyrethrum-based emulsifiable larvicide. The emulsion concentrate contains 0.1 to 0.2 per cent pyrethrins by weight and is required to be diluted with water before use. The emulsion is diluted in the ratio of 1 :4, (c) Organophosphorus larvicides : During the past 10 years, organophosphorus larvicides (e.g., temephos, fenthion) have been widely used with successful results.
In the case of Mansonia mosquitoes, breeding is best controlled by removing the supporting aquatic vegetation such as the pistia plant from all water collections and converting the ponds to fish or lotus c,:ulture. Alternatively, certain herbicides such as phenoxylene 30 or Shell Weed Killer D may be used for destroying the aquatic vegetation.
 Users Today : 8
Users Today : 8 Users Yesterday : 2
Users Yesterday : 2 Users Last 7 days : 20
Users Last 7 days : 20 Users Last 30 days : 71
Users Last 30 days : 71 Users This Month : 71
Users This Month : 71