Leptospirosis is essentially animal infection by several serotypes of Leptospira (Spirocheates) and transmitted to man under certain environmental conditions. The disease manifestations are many and varied, ranging in severity from a mild febrile illness to severe, and sometimes fatal disease with liver and kidney involvement.
AGENT FACTORS :
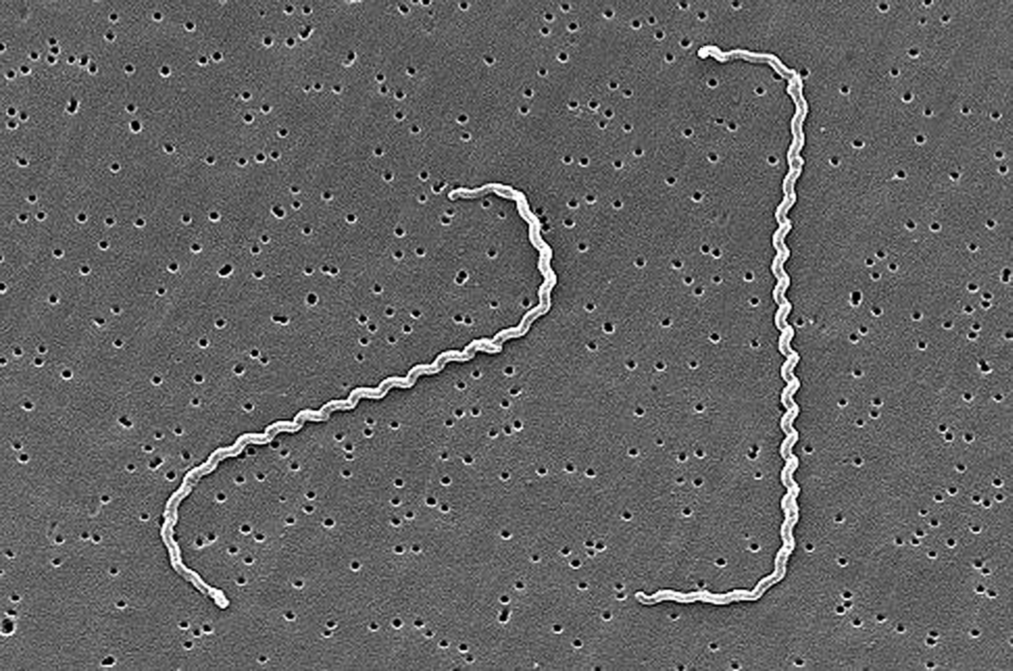
Leptospira are thin and light motile spirocheates 0.1-0.2 μm wide and 5-15 μm long with hooked ends. The organisms are visible by dark-field illumination and silver staining.
SOURCE OF INFECTION :
Leptospira are excreted in the urine of infected animals for a long time, often for an entire life time in cases of rodents. Leptospirosis affects wild and domestic animals worldwide especially rodents such as rats, mice and voles. Most domestic animals including cattle, sheep, goats, water buffalo, pigs and horses may be infected through grazing in areas contaminated by the urine of the carrier host. Rats and small rodents – particularly R. norvegicus and Mus musculus are the most important reservoirs.
HOST FACTORS :
Children acquire the infection from dogs more frequently than do adults. Human infection is only accidental. Human infections are usually due to occupational exposure to the urine of infected animals, e.g, agricultural and livestock farmers, workers in rice fields, sugarcane fields, and underground sewers, abattoir workers, meat and animal handlers, veterinarians etc. Leisure time activities such as swimming and fishing may also carry risks.
Mode of transmission :

DIRECT CONTACT :
Leptospira can enter the body through skin abrasions or through intact mucous membrane by direct contact with urine or tissue of infected animal.
INDIRECT CONTACT :
Through the contact of the broken skin with soil, water or vegetation contaminated by urine of infected animals or through ingestion of food or water contaminated with leptospirae.
DROPLET INFECTION :
Infection may also occur through inhalation as when milking infected cows or goats by breathing air polluted with droplets of urine.
INCUBATION PERIOD :
Usually 10 days with a range of 4 to 20 days.
DIAGNOSIS :
Early in the disease, the organism may be identified by dark-field examination of the patient’s blood or by culture on a semisolid medium. Culture takes 1-6 weeks to become positive. The organism may also be grown from the urine from 10th day to 6 weeks. Diagnosis is usually made by means of serological tests, of which several are available. Agglutination tests (microscopic using live organism, and macroscopic using killed antigen) become positive after 7-10 days of illness and peak at 3-4 weeks and may persist at high level for many years. Indirect haemagglutination, immunoflourescent antibody and ELISA tests are also available. The IgM ELISA is particularly useful in making an early diagnosis, as it is positive as early as 2 days into illness.
CONTROL :
ANTIBIOTICS : Penicillin is the drug of choice but other antibiotics (tetracycline or doxycycline) are also effective. The dosage of penicillin is 6 million units daily intravenously.
ENVIRONMENTAL MEASURES : This includes preventing exposure to potentially contaminated water,
reducing contamination by rodent control and protection of workers in hazardous occupation. Measures should be taken to control rodents, proper disposal of wastes and health education.
VACCINATION :
Immunization of farmers and pets prevent disease. In some countries for instance Italy, USSR and China, where certain occupations carry a high risk of infection, vaccines are available.
 Users Today : 2
Users Today : 2 Users Yesterday : 3
Users Yesterday : 3 Users Last 7 days : 18
Users Last 7 days : 18 Users Last 30 days : 103
Users Last 30 days : 103 Users This Month : 74
Users This Month : 74