
An acute disease induced by the exotoxin of Clostridium tetani and clinically characterized by muscular rigidity which persists throughout illness punctuated by painful paroxysmal spasms of the voluntary muscles, especially the masseters (trismus or “lock-jaw”), the facial muscles (risus sardonicus), the muscles of the back and neck (opisthotonos), and those of the lower limbs and abdomen.
AGENT:
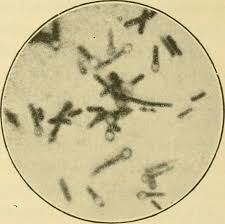
Cl. tetani is a gram-positive, anaerobic, spore-bearing organism. The spores are present on distal end therefore it looks like drumsticks.
RESERVOIR OF INFECTION:
The natural habitat of the organism is soil and dust. The bacilli are found in the intestine of many herbivorous animals, e.g., cattle, horses, goats and sheep and are excreted in their faeces. The spores survive for years in nature. The bacilli may be found frequently in the intestine of man without causing ill effects.
EXOTOXIN:
Tetanus bacilli produce a soluble exotoxin. It has an more lethal toxicity, greater than only by botulinum toxin. for a 70 kg man the lethal dose is about 0 .1 mg. The toxin acts on 4 areas of the nervous system :
- the motor end plates in skeletal system
- the spinal cord
- the brain,
- the sympathetic system. Its principal action is to block inhibition of spinal reflexes
PERIOD OF COMMUNICABILITY:
Not transmitted from person to person.
Host factors:
AGE:

Tetanus mostly found in active age group of 5yrs to 40yrs. This period predisposes to all kinds of trauma and therefore, the risk of acquiring the disease is pretty high. “neonatal tetanus” is tetanus occurring in the new-born.
SEX:
Females are more exposed to the risk of tetanus, although a higher incidence is found in males, especially during delivery or abortion leading to “puerperal tetanus”.
OCCUPATION:
Agriculture workers, labours, outdoor worker are at high incidence of tetanus.
RURAL-URBAN DIFFERENCES:
The incidence of tetanus is much lower in urban than in rural areas. Within the urban areas, there may be vast differences in the incidence of tetanus. It is seen that tetanus prevalance is more outskirt of town where floor is not made up of firm base than center of town where mosaic tiles are used.
IMMUNITY:
No age is immune unless protected by previous immunization. The immunity resulting from 2 injections of tetanus toxoid is highly effective and lasts for several years.
Mode of transmission:

Contamination of tetanus spore in open wound causes tetanus. Following injuries lead to tetanus consist of a trivial pin prick, skin, abrasion, puncture wounds, burns, human bites, animal bites and stings, unsterile surgery, intra-uterine death, bowel surgery, dental extractions, injections, unsterile division of umbilical cord, compound fractures, otitis media, chronic skin ulcers, eye infections, and gangrenous limbs.
Incubation period:
The incubation period is usually 6 to 10 days.
Types of tetanus:
TRAUMATIC:
Trauma is a major and important cause of tetanus. In few incidence unnoticed wound causes tetanus.
PUERPERAL:
Tetanus follows abortion more frequently than a normal labour.
OTOGENIC:
Ear may be a rare portal of entry. External object like infected pencils, sticks can cause otogenic tetanus.
IDIOPATHIC:

In these cases there is no definite history of sustaining an injury. Some consider it to be the result of microscopic trauma.
TETANUS NEONATORUM:
The common cause is infection of the umbilical stump after birth, the first symptom being seen about the 7th day. Therefore tetanus is known as “8th day disease”.
PREVENTION:
Active immunization:
Active immunization is best mode to prevent tetanus. It stimulates the production of the protective antitoxin. Two preparations are available for active immunization:
- Combined vaccine – DPT
- Monovalent vaccines
COMBINED VACCINE:
Tetanus vaccine is offered routinely to infants (Expanded Immunization Programme} in combination with diphtheria vaccine and killed B. pertussis organisms as DPT vaccine.
MONOVALENT VACCINES:

Purified tetanus toxoid (adsorbed) has largely supplanted plain toxoid because it stimulates a higher and longer lasting immunity response than plain toxoid.
Two doses of tetanus toxoid adsorbed (each dose 0.5 ml, injected into the arm) given at intervals of 1-2 months is a primary course of immunization. The longer the intervals between the two doses, the better is the immune response.
Passive immunization:

Temporary protection against tetanus can be provided by an injection of human tetanus hyperimmunoglobulin (TIG).
Active and passive immunization:
The purpose of antitoxin is for immediate temporary protection, and the purpose of toxoid is for long-lasting protection.
Antibiotics:
A long acting penicillin which maintain there concentration in plasma for 3 to4 weeks, is sufficient to kill any vegetative forms of tetanus bacilli that may emerge from the sporulating stage.
Prevention of neonatal tetanus:
Neonatal tetanus is well controlled in some industrialized countries through clean delivery practices alone. Most programmes in developing countries have concentrated on training the traditional birth attendants, providing home delivery kits and educating pregnant women about the “three cleans” – clean hands, clean delivery surface and clean cord care i.e., clean blade for cutting the cord, clean tie for the cord and no application on the cord stump.
In unimmunized pregnant women, two doses of tetanus toxoid should be given, the first as early as possible during pregnancy and the second at least a month later and at least 3 weeks before delivery. In areas where the incidence of neonatal tetanus is high, the primary 2-dose course can be extended to all women of child-bearing age, particularly if the present coverage of antenatal care is low.
Prevention of tetanus after injury:

All wounds must be thoroughly cleaned soon after injury removal of foreign bodies, soil, dust, necrotic tissue. This procedure can cause transfer of tetanus spore in wound if not done with starile precautions.
Wounds less than 6 hours old, clean, non-penetrating and with negligible tissue damage:
| Immunity category | Treatment |
| A | Nothing more required |
| B | Toxoid 1 dose |
| C | Toxoid 1 dose |
| D | Toxoid complete course |
Other wounds:
| Immunity category | Treatment· |
| Nothing more required | |
| Toxoid 1 dose | |
| Toxoid 1 dose + Human Tet. lg | |
| Toxoid complete course + Human Tet. lg |
A = Has had a complete course of toxoid or a booster dose within the past 5 years.
B = Has had a complete course of toxoid or a booster dose more than 5 years ago and less than 10 years ago.
C = Has had a complete course of toxoid or a booster dose more than 10 years ago.
D = Has not a complete course of toxoid or immunity status is unknown.
 Users Today : 2
Users Today : 2 Users Yesterday : 3
Users Yesterday : 3 Users Last 7 days : 18
Users Last 7 days : 18 Users Last 30 days : 103
Users Last 30 days : 103 Users This Month : 74
Users This Month : 74