
Acute respiratory infections (ARI) may cause inflammation of the respiratory tract anywhere from nose to alveoli, with a wide range of combination of symptoms and signs. Acute respiratory infection is often divided on the basis of location of infection. if infection occur in upper respiratory tract it is called as upper ARI and if infection occur at lower respiratory tract it is called as lower ARI. Common cold, pharyngitis, and otitis media come under the upper respiratory tract infections. Epiglottitis, laryngitis, laryngo-tracheitis, bronchitis, bronchiolitis and pneumonia are come under the lower respiratory tract infection.
Agent factors:
There are various bacterias and viruses responsible for causing acute respiratory infections in body. Even within species they can show a wide diversity of antigenic type.
Host factors:
Upper respiratory tract infections, e.g., common cold and pharyngitis are several times higher in children than in, adults. Rates for pharyngitis and otitis media increase from infancy to a peak at the age of 5 years.
Mode of transmission:

All the causative organisms are normally transmitted by the airborne route. As most viruses do not survive for long outside the respiratory tract, the chain of transmission is maintained by direct person-to-person contact.
Classification of Illness:
Classifying the illness is helpful in differentiate type and severity of disease. The sick child should be put into one of the four classifications:
- Very severe disease
- Severe pneumonia
- Pneumonia (not severe}
- No pneumonia: cough or cold
Very severe disease:
The danger signs and possible causes are :
- Not able to drink : A child who is not able to drink could have severe pneumonia or bronchiolitis, septicemia, throat abscess, meningitis or cerebral malaria.
- Convulsions, abnormally sleepy or difficult to wake : A child with these signs may have severe pneumonia resulting in hypoxia, sepsis, cerebral malaria or meningitis. Meningitis can develop as a complication of pneumonia or it can occur on its own.
- Strider in calm child: If a child has strider when calm, the child may be in danger of life-threatening obstruction of the air-way from swelling of larynx, trachea or epiglottis.
- Severe malnutrition: A severely malnourished child is at high risk of developing and dying from pneumonia. In addition, the child may not show typical signs of the illness.
Severe pneumonia:

Childs respiratory rate and chest indrawing are most helpful to deciding whether child has pneumonia or not. If the effort needed to expand of lungs is more then, chest indrawing is seen but fast breathing may not seen because of exhaustion of child. Some children with chest indrawing also have wheezing. Severe pneumonia is consider when there is chest indrawing and a first episode of wheezing.
- A child classified as having severe pneumonia also has other signs such as:
- nasal flaring, when the nose widens as the child breaths in;
- grunting, the short sounds made with the voice when the child has difficulty in breathing; and
- cyanosis, a dark bluish or purplish coloration of the skin caused by hypoxia.
Pneumonia (not severe):
Only fast breathing without chest indrawing are consider as pneumonia (not severe). If children brought early for treatment then these are consider in above catagory.
No pneumonia: cough or cold
Most children with a cough or difficult breathing do not have any danger signs or signs of pneumonia (chest indrawing or fast breathing). These children have a simple cough or cold. Cold mostly cover within 7-14 days. However, a child with chronic cough (lasting more than 30 days) may have tuberculosis, asthma, whooping cough or some other problem.
Management of acute respiratory infections:
| SIGNS | Not able to drink, Convulsions Abnormally sleepy or difficult to wake Stridor in calm child, or Severe malnutrition | Chest indrawing (if also recurrent wheezing go directly to treat wheezing) | No chest indrawing and , fast breathing (50 per minute or more if child 2 months upto 12 months; 40 per minute or more if child 12 months upto 5 years | No chest indrawing and No fast breathing (Less 50 per minute if child 2 months up to 12 months; than 40 per minute if child is 12 months up to 5 years). |
| CLASSIFY AS | VERY SEVERE DISEASE | SEVERE PNEUMONIA | PNEUMONIA | NO PNEUMONIA: COUGH OR COLD |
| TREATMENT | Give first dose of an antibiotic Treat fever, if present Treat wheezing, if present If cerebral malaria i,;> possible, give an antimalarial | Refer URGENTLY to hospital Give first dose of an antibiotic Treat fever, if present, Treat fever, if present, Treat wheezing, if present (if referral is not feasible, treat with an antibiotic and follow closely) | Advise mother to give home care. Give an antibiotic. Treat fever, if present. Treat wheezing, if present. Advise mother to return with child in 2 days for reassessment, or earlier if the child is getting worse. | If coughing more than 30 days, refer for assessment. Assess and treat ear problem or sore throat, if present. Assess and treat other problems. Advise mother to give home care. Treat fever, if present. Treat wheezing, if present. |
Treatment:

TREATMENT FOR CHILDREN AGED 2 MONTHS UPTO 5 YEARS:
The standard treatment for childhood acute respiratory infections in India is as follows:
PNEUMONIA (CHILD WITH COUGH AND FAST BREATHING):
| AGE/WEIGHT | Paediatric tablet : Sulphamethoxazole 100 mg and Trimethoprim 20 mg | Paediatric syrup : Each spoon (5 ml) : Sulphamethoxazole 200mg and Trimethoprim 40 mg |
| < 2 months (Wt. 3-5 kg) | One tablet twice a day | Half spoon (2.5 ml) twice a day |
| 2-12 months (Wt. 6-9 kg) | Two tablets twice a day | One spoon (5 ml) twice a day |
| 1-5 years (Wt. 10-19 kg) | Three tablets twice a day | One. and half spoon (7.5 ml) twice a day. |
SEVERE PNEUMONIA (CHEST IN-DRAWING):
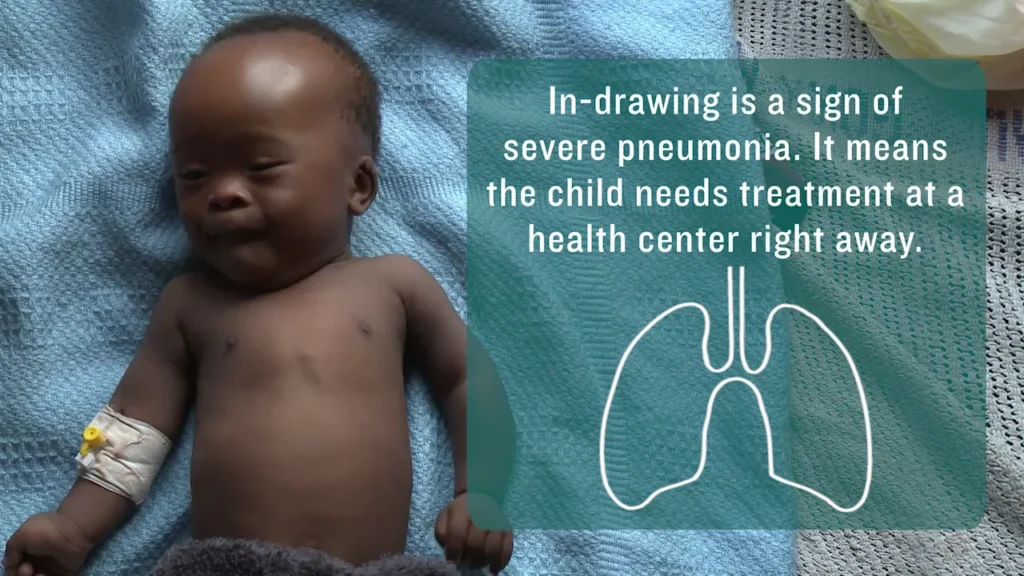
Children with severe pneumonia should be treated as inpatients with intramuscular injections of benzyl penicillin (after test dose), ampicillin or chloramphenicol. The condition of child must checked every day and review after 2 days of antibiotic treatment.
VERY SEVERE DISEASE:
Children with signs of very severe disease are in imminent danger of death, and should be treated in a health facility, with provision for oxygen therapy and intensive monitoring. Chloramphenicol IM is the drug of choice in all such cases. After 48 hours if condition improve switch over to chloramphenicol. Chloramphenicol should be given for a total of 10 days. If condition worsens or does not improve after 48 hours, switch to IM injections of cloxacillin and gentamycine.
NO PNEUMONIA:
Many children with presenting symptoms of cough, cold and fever do not have pneumonia (no fast breathing or chest indrawing) and DO NOT require treatment with antibiotics.
Immunization:

Below three vaccines are useful in pneumonia.
MEASLES VACCINE:
If we reduce measles by using measles vaccine it will be helpful to reduce pneumonia.
HIB VACCINE:
Heamophelus influenza is also helpful to reduce the cases of pneumonia by using HIB vaccines in developing countries.
PNEUMOCOCCAL PNEUMONIA VACCINE:
PPV23:
Children under 2 years of age and immunocompromised individuals do not respond well to the vaccine. It is recommended for selected groups.
PCV:
Two conjugate vaccines are available since 2009 PCV10 and PCV13• The PCV7 conjugate vaccine is
gradually being removed from the market.

 Users Today : 0
Users Today : 0 Users Yesterday : 2
Users Yesterday : 2 Users Last 7 days : 13
Users Last 7 days : 13 Users Last 30 days : 65
Users Last 30 days : 65 Users This Month : 57
Users This Month : 57