
Typhoid fever is the result of systemic infection mainly by S. typhi found only in man. The disease is clinically characterized by a typical continuous fever for 3 to 4 weeks relative bradycardia with involvement of lymphoid tissue and considerable constitutional symptoms. The term “enteric fever” includes both typhoid and paratyphoid fevers.
Typhoid fever occurs in all parts of the world where water supplies and sanitation are sub-standard. The socio-economic impact of the disease is huge, because typhoid survivors may take several months to recover and resume work.
Agent factors:
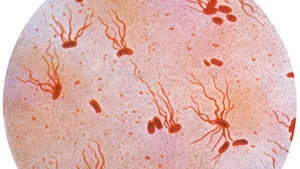
S. typhi is the major cause of enteric fever. S. para A and S. para Bare relatively infrequent. S. typhi has three main antigens 0, H and Vi and a number of phage types at least 80. Man is the only known reservoir of infection.
Cases:
The case may be mild, missed or severe. A case (or carrier) is infectious as long as bacilli appear in stools or urine.
Carriers:
The carriers may be temporary (incubatory, convalescent) or chronic. Convalescent carriers excrete the bacilli for 6 to 8 weeks, after which their numbers diminish rapidly. By the end of three months, not more than 4 per cent of cases are still excreting the organisms; and by the end of one year, the average carrier rate is around 3 per cent.
Source Of Infection:
The primary sources of infection are faeces and urine of cases or carriers; the secondary sources contaminated water, food, fingers and flies.
Incubation period:
Usually 10-14 days. But it may be as short as 3 days or as long as three weeks depending upon the dose of the bacilli ingested.
Modes of transmission:
Typhoid fever is transmitted via the faecal-oral route or urine-oral routes. This may take place directly through soiled hands contaminated with faeces or urine of cases or carriers, or indirectly by the ingestion of contaminated water, milk and/or food, or through flies.
Clinical features:
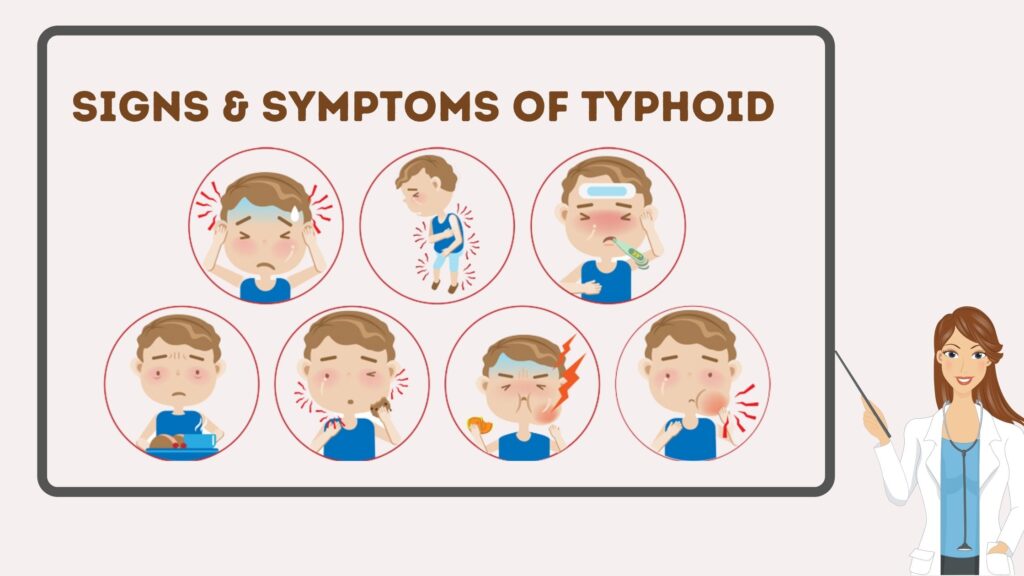
The onset is usually insidious but in children may be abrupt, with chills and high fever. During the prodromal stage, there is malaise, headache, cough and sore throat, often with abdominal pain and constipation. The fever ascends in a step-ladder fashion. After about 7-10 days, the fever reaches a plateau and the patient looks toxic, appearing exhausted and often prostrated. There may be marked constipation, especially in early stage or “pea soup” diarrhoea.
During the early phase, physical findings are few. Later, splenomegaly, abdominal distension and tenderness, relative bradycardia, dicrotic pulse, and occasionally meningismus appear. The individual spot, found principally on the trunk, is a pink papule 2-3 mm in diameter that fades on pressure. It disappears in 3-4 days.
Intestinal haemorrhage is manifested by a sudden drop in temperature and signs of shock, followed by dark or fresh blood in the stool. Intestinal perforation is most likely to occur during the third week. Less frequent complications are urinary retention, pneumonia, thrombophlebitis, myocarditis, psychosis, cholecystitis, nephritis and osteomyelitis.
Laboratory diagnosis of typhoid:
Microbiological Procedures :
The definitive diagnosis of typhoid fever depends on the isolation of S. typhi from blood, bone marrow and stools.
Serological Procedures:
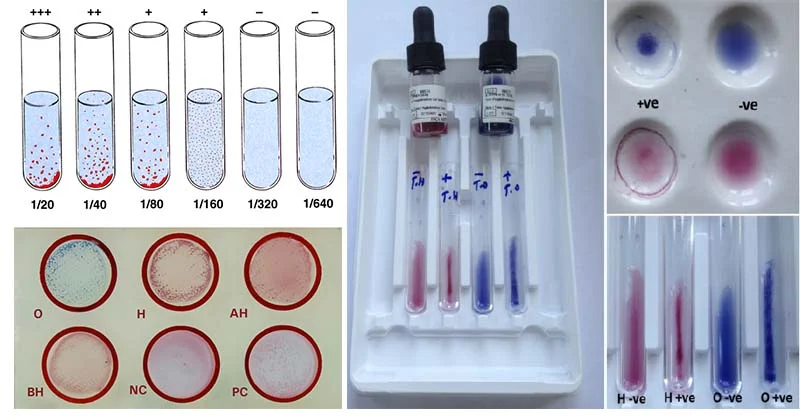
Felix-Widal Test measures agglutinating antibody levels against 0 and H antigens. Usually, 0 antibodies appear on day 6-8 and H antibodies on day 10-12 after the onset of disease.
New Diagnostics Tests:
The recent advances for quick and reliable diagnostic tests for typhoid fever as an alternative to the Widal test include the IDL Tubex test marketed by a Swedish company, which reportedly can detect lgM09 antibodies from patient within a few minutes. Another rapid serological test, Typhidot, takes three hours to perform.
Carriers:

Since carriers are the ultimate source of typhoid fever, their identification and treatment is one of the most radical ways of controlling typhoid fever. Carriers are identified by cultural and serological examinations. The carrier should be given an intensive course of ampicillin or amoxycillin (4-6 g a day} together with Probenecid (2 g/day) for 6 weeks.
Treatment of uncomplicated typhoid fever:

| Susceptibility | Antibiotics |
| Fully sensitive | Fluoroquinolones. |
| Multidrug resistance | Fluoroquinolones or Cefixime. |
| Quinolone resistance | Azithromycin or Ceftriaxone. |
Control of sanitation:
Protection and purification of drinking water supplies, improvement of basic sanitation, and promotion of food hygiene are essential measures to interrupt transmission of typhoid fever.
Immunization:

Control of typhoid fever must take the form of improved sanitation and domestic and personal hygiene, these are long-term objectives in many developing countries. It can be given at any age upwards of two years. It is recommended to :
- those living in endemic areas.
- household contacts.
- groups at risk of infection such as school children and hospital staff.
- travellers proceeding to endemic areas.
- those attending me/as and yatras.
ANTI-TYPHOID VACCINES:
The old parenteral killed whole-cell vaccine was effective but produced strong side-effects, Two safe and effective vaccines are now licensed and available.
The Vi polysaccharide vaccine:
The vaccine is licensed for individuals aged 2 years. Only 1 dose is required, and the vaccine confers protection 7 days after injection. To maintain protection, revaccination is recommended every 3 years.
The Ty2 la vaccine:
The vaccine is administered every other day; on 1, 3, and 5th day; a 3-dose regimen is recommended. With the 3-dose regimen, protective immunity is achieved 7 days after the last dose.

 Users Today : 2
Users Today : 2 Users Yesterday : 3
Users Yesterday : 3 Users Last 7 days : 18
Users Last 7 days : 18 Users Last 30 days : 103
Users Last 30 days : 103 Users This Month : 74
Users This Month : 74