
Dengue viruses are arboviruses capable of infecting humans, and causing disease. These infections may be asymptomatic or may lead to:
- “classical” dengue fever,
- dengue hemorrhagic fever without shock,
- dengue hemorrhagic fever with shock.
A prevalence of Aedes aegypti and Aedes albopictus together with the circulation of dengue virus of more than one type in any particular area tends to be associated with outbreaks of DHF/DSS.
Epidemiology:
In India, the risk of dengue has shown an increase in recent years due to rapid urbanization, lifestyle changes and deficient water management including improper water storage practices in urban, peri-urban and rural areas, leading to proliferation of mosquito breeding sites.
Agent:
The dengue virus form a distinct complex within the genus flavivirus based on antigenic and biological characteristics. There are four virus serotypes which are designated as DENV-1, DENV-2, DENV-3 and DENV-4. Infection with any one serotype confers lifelong immunity to that virus serotype. Secondary infection with dengue serotype 2 or multiple infection with different serotypes lead to severe form dengue DHF/DSS.
Vector:

Aedes aegypti and Aedes Albopictus arethe two most important vectors of dengue. They both carry high vectoral competency for dengue virus, i.e., high susceptibility to infecting virus, ability to replicate the virus and ability to transmit the virus to another host.
Transmission of disease:
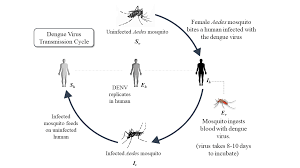
The Aedes mosquito becomes infective by feeding on a patient from the day before onset to the 5th day (viremia stage) of illness. After an extrinsic incubation period of 8 to 10 days, the mosquito becomes infective, and is able to transmit the infection.
The population of Aedes aegypti fluctuates with rainfall and water storage. Its life span is influenced by temperature and humidity, survives best between 16°C-30°C and a relative humidity of 60-80 per cent. It breeds in the containers in and around the houses.
Dengue in community:
A number of factors that contribute to initiation and maintenance of an epidemic include:
- the strain of the virus
- the density, behaviour and vectoral capacity of the vector population;
- the susceptibility of the human population
- the introduction of the virus into a receptive community.
High risk patients:

The following host factors contribute to more severe disease and its complications:
- infants and elderly ;
- obesity;
- pregnancy;
- peptic ulcer disease;
- women who are in menstruation or have abnormal bleeding;
- hemolytic disease such as G-6PD, thalassemia and other haemoglobinopathies;
- congenital heart disease;
- chronic diseases such as diabetes mellitus, hypertension, asthma, ischemic heart disease, chronic renal failure, liver cirrhosis; and
- patients on steroid or NSAID treatment.
Clinical manifestation:
Dengue virus infection may be asymptomatic or may cause undifferentiated febrile illness (viral syndrome}, dengue fever(DF), or dengue hemorrhagic fever (DHF} including dengue shock syndrome (DSS}.
Undifferentiated fever:
Infants, children and adults who have been infected with dengue virus, especially for the first time may develop a simple fever indistinguishable from other viral infection. Maculopapular rashes may accompany the fever.
Classical dengue fever:
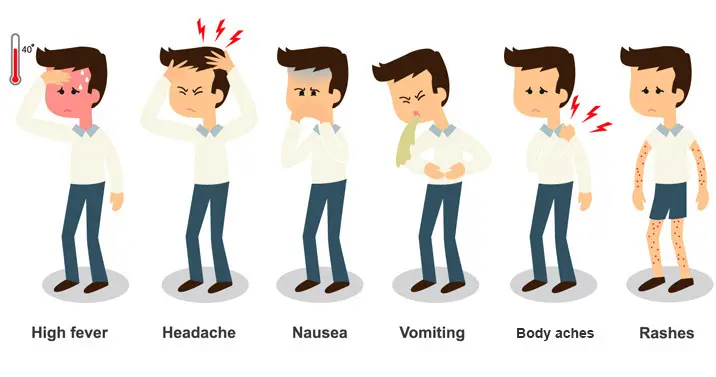
The illness is characterized by an incubation period of 3 to 10 days. The onset is sudden, with chills and high fever, intense headache, muscle and joint pains, which prevent all movement. Within 24 hours retro-orbital pain, particularly on eye movements or eye pressure and photophobia develops. Other common symptoms include extreme weakness, anorexia, constipation, altered taste sensation, colicky pain and abdominal tenderness, dragging, pain in inguinal region, sore throat and general depression. Fever is usually between 39°C and 40°C.
Dengue hemorrhagic fever:
Dengue haemorrhagic fever (DHF) is a severe form of dengue fever. The course of dengue illness can be divided into three phases-febrile phase, critical phase and recovery phase.
Febrile phase:
Following an incubation period of four to six days, the illness commonly begins abruptly with high fever accompanied by facial flushing and headache. Anorexia, vomiting, epigastric discomfort, tenderness at the right costal margin and generalized abdominal pain are common.
The major pathophysiologic changes that determine the severity of disease in DHF and differentiate it from OF are plasma leakage and abnormal hemostasis, as manifested by a rising hematocrit value and moderate to marked thrombocytopenia. A positive tourniqute test is the most common hemorrhagic phenomenon.
Critical phase:

Around the time of defervescence, when the temperature drops to 37.5-38°C or less, and remains below this level, usually on days 3-7 of illness, an increase in capillary permeability in parallel with increasing haematocrit levels may occur. This marks the beginning of the critical phase. The period of clinically significant plasma leakage usually lasts 24-48 hours.
Progressive leukopenia followed by a rapid decrease in platelet count usually precedes plasma leakage. Shock occurs when a critical volume of plasma is lost through leakage. It is often preceded by warning signs of abdominal pain or tenderness, persistent vomiting.
Recovery phase:
If the patient survives the 24-48 hour critical phase, a gradual reabsorption of extravascular compartment fluid takes place in the following 48-72 hours. Respiratory distress from massive pleural effusion and ascites will occur at any time if excessive intravenous fluids have been administered.
CRITERIA FOR CLINICAL DIAGNOSIS:
Dengue fever:
Probable diagnosis:
- Acute febrile illness with two or more of the following;
- headache,
- retro-orbital pain,
- myalgia,
- arthralgia/bone pain,
- rash,
- haemorrhagic manifestations,
- leucopenia (wbc s 5000 cells/mm3),
- thrombocytopenia (platelet count <150,000 cells/mm3),
- rising hematocrit (5-10%);
Dengue hemorrhagic fever:

Acute onset of fever of two to seven days duration. hemorrhagic manifestations, shown by any of the following; positive tourniquet test, petechiae, ecchymoses or purpura, or bleeding from mucosa, gastrointestinal tract, injection sites, or other locations. Platelet count S: 100,000 cells/mm3.
Dengue shock syndrome:
Criteria for dengue hemorrhagic fever as above with signs of shock including:
- tachycardia, cool extremities, delayed capillary refill, weak pulse, lethargy or restlessness, which may be a sign of reduced brain perfusion.
- pulse pressure ~ 20 mmHg with increased diastolic pressure, e.g. 100/80 mmHg.
- hypotension by age, defined as systolic pressure <80 mmHg for those aged <5 years, or SO to 90 mmHg for older children and adults.
Clinical Management:
A haematocrit test in the early febrile phase establishes the patient’s own baseline haematocrit. A rapidly decreasing platelet count in parallel with a rising haematocrit compared to the baseline is suggestive of progress to the plasma leakage/critical phase of the disease.
Management of dengue fever:

- Encourage intake of oral rehydration solution (ORS), fruit juice and other fluids containing electrolytes and sugar to replace losses from fever and vomiting.
- Give paracetamol for high fever if the patient is uncomfortable.
- Instruct the care-givers that the patient should be brought to hospital immediately if any of the following occur; no clinical improvement, deterioration around the time of defervescence, severe abdominal pain, persistent vomiting, cold and clammy extremities, lethargy or irritability/ restlessness, bleeding, not passing urine for more than 4-6 hours.
Management of DHF:
Patients should be closely monitored for the initial signs of shock. The critical period is during the transition from the febrile to the afebrile stage and usually occurs after the third day of illness. Hematocrit should be determined daily from the third day until the temperature has remained normal for one or two days.
Indications of red cell transfusion:

- Loss of blood (overt blood) – 10 per cent or more of total blood volume – preferably give whole blood or components to be used.
- Refractory shock despite adequate fluid administration and declining hematocrit.
Indications of platelet transfusion:
In general there is no need to give prophylactic platelet even at< 20,000/cu.mm.
Criteria for discharge of patients:
- Absence of fever for at-least 24 hours without the use of anti-pyretic drugs.
- Return of appetite.
- Visible clinical improvement.
- Good urine output.
- Minimum of 2-3 days after recovery from shock.
- No respiratory distress from pleural effusion or ascites.
- Platelet count> 50,000/cu.mm.
 Users Today : 2
Users Today : 2 Users Yesterday : 3
Users Yesterday : 3 Users Last 7 days : 18
Users Last 7 days : 18 Users Last 30 days : 103
Users Last 30 days : 103 Users This Month : 74
Users This Month : 74