
Rabies, also known as hydrophobia is an acute, highly fatal viral disease of the central nervous system, caused by Lyssavirus type 1. It is primarily a zoonotic disease of warm blooded animals, particularly carnivorous such as dogs, cats, jackals and wolves. It is transmitted to man usually by bites or licks of rabid animals. Classical hydrophobia is clinically characterized by a long and variable incubation period, a short period of illness due to encephalomyelitis ending in death, despite intensive care. It is the only communicable disease of man that is always fatal.
Causative agent:
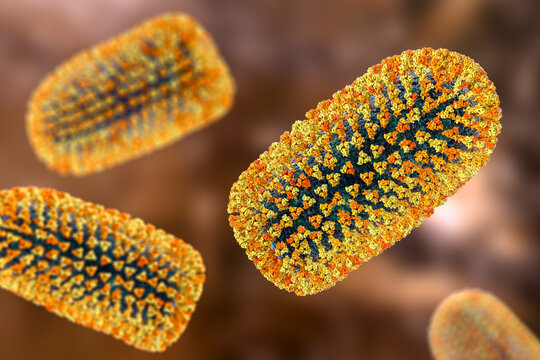
The causative agent (Lyssavirus type 1) is a bullet shaped neurotropic RNA containing virus. It belongs to the family rhabdoviridae – serotype 1 (Lyssavirus, type 1) and is the causative agent of rabies. Serotype 2, 3 and 4 are rabies-related but antigenically distinct viruses; they cause rabies like disease in man and animals. Available antirabies vaccines may not be effective against the rabies related viruses.
Transmission of disease:

Animal bite category:
- Type 1: Licks – no tissue injury – wound management
- Type 2: Abrasion/ Laceration – wound management +ARV
- Type 3: wound management +ARV+ Rabies immunoglobulin
wild animal bite: always type 3
Bats are the source of most human rabies deaths in the United States of America and Canada. Rarely, rabies may be contracted by inhalation of virus containing aerosol or via transplantation of an infected organ.
Incubation period:
The incubation period in man is highly variable, commonly 1-3 months following exposure but may vary from 7 days to many years. The incubation period depends on the site of the bite, severity of the bite, number of wounds, amount of virus injected, species of the biting animal, protection provided by the clothing and treatment undertaken, if any.
Pathogenesis of rabies:
Rabies virus replicates in muscle or connective tissue cells at or near the site of introduction before it attaches to nerve endings and enters peripheral nerves. It spreads from the site of infection centripetally via the peripheral nerves towards the central nervous system; most likely it “ascends” passively through the nerve associated tissue space.
Clinical presentation:

The disease begins with prodromal symptoms such as headache, malaise, sore throat and slight fever lasting for 3-4 days. The patient is intolerant to noise, bright light or a cold draught of air (sensory). Aerophobia (fear of air) may be present. Mental changes include fear of death, anger, irritability and depression. At later stage the mere sight or sound of water may provoke spasm of the muscles of deglutition. The duration of illness is 2 to 3 days, but may be prolonged to 5-6 days in exceptional cases. The patient may die abruptly during one of the convulsions or may pass on to the stage of paralysis and coma.
Investigation:
Rabies can be confirmed in patients early in the illness by antigen detection using immunofluorescence of skin biopsy, and by virus isolation from saliva and other secretions.
Treatment:
There is no specific treatment for rabies. The patient should be isolated in a quiet room protected as far as possible from external stimuli such as bright light, noise or cold draughts which may precipitate spasms or convulsions. Nursing personnel attending rabid patients should be warned against possible risk of contamination and should wear face masks, gloves, goggles and aprons to protect themselves. Persons having bruises, cuts or open wounds should not be entrusted to look after the patient.
Immunization:

This may be considered under 3 heads.
- a. Post-exposure prophylaxis.
- b. Pre-exposure prophylaxis.
- c. Post-exposure treatment of persons who have been vaccinated previously.
Post-exposure prophylaxis:
The aim of post-exposure prophylaxis is to neutralize the inoculated virus before it can enter the nervous system. Every instance of human exposure should be treated as a medical emergency.
Local treatment of wound:
The purpose of local treatment is to remove as much virus as possible from the site of inoculation before it can be absorbed on nerve endings.
Cleansing:
Immediate flushing and washing the wound(s), scratches and the adjoining areas with plenty of soap and water, preferably under a running tap, for at least 15 minutes is of paramount importance in the prevention of human rabies.
Chemical treatment :
Whatever residual virus remains in the wound(s), after cleansing, should be inactivated by irrigation with virucidal agents either alcohol (400-700 ml/litre), tincture or 0.01 % aqueous solution of iodine or povidone iodine.
Suturing:
Bite wounds should not be immediately sutured to prevent additional trauma which may help spread the virus into deeper tissues.
Post exposure prophylaxis:

IPC Schedule:
Intradermal, 2 site schedule.
| Day | 0 | 3 | 7 |
| Dose | 2 | 2 | 2 |
Modified Essen Schedule:
IM one site.
| Day | 0 | 3 | 7 | 14-28 |
| Dose | 1 | 1 | 1 | 1 |
Modified Zagreb schedule:
| Day | 0 | 3 | 7 | 14 | 21 |
| Dose | 2 | 0 | 1 | 0 | 1 |
Thai red cross schedule:
| Day | 0 | 3 | 7 | 14 | 21 | 28 |
| Dose | 2 | 2 | 2 | 0 | 0 | 2 |
Pre exposure prophylaxis:
0,7 days – ID 2 site.
0,7 days – IM 1 site.
Re-exposure prophylaxis:
ID 1 site- day 0,3.
IM 1 site- day 0,3.
ID 4 site- day 0.
Rabies Immunoglobulin:

The dose of human rabies immunoglobulin is 20 IU/kg body weight; for equine immunoglobulin and F (ab’)2 products, it is 40 IU/kg body weight.
Rabies in dog:
In developing countries over 903 of human deaths from rabies are caused by dog bites and dog rabies control is the key that can lock the door against human rabies.
Incubation Period:
The incubation period in dogs ranges from 3-8 weeks, but it may be as short as 10 days or as long as a year or more.
Clinical features:

Furious rabies:
This is the typical “mad-dog syndrome”, characterized by
- a change in behaviour : In animals, the cardinal sign is a change in behaviour. The animal loses its fear of people, becomes very aggressive, bites without provocation.
- running amuck: i.e., tendency to run away from home and wander aimlessly and biting humans and animals who may come in its way.
- Change in voice : i.e., the dog barks or growls in a hoarse voice or often unable to bark because of paralysis of laryngeal muscles.
- excessive salivation and foaming at the angle of the mouth.
- Paralytic stage : The animal enters into a paralytic stage, towards the later stages of illness.
Dumb rabies :
In this type, the excitative or irritative stage is lacking. The disease is predominantly paralytic.
Investigations:
The head of the animal is cut off and sent to the nearest testing laboratory, duly packed in ice in an airtight container.
- FLUORESCENT ANTIBODY TEST : This is a highly reliable and the best single test currently available for the rapid diagnosis of rabies viral antigen in infected specimens.
- MICROSCOPIC EXAMINATION: Although FRA test has largely supplanted other methods of diagnosis, the microscopic examination of brain tissue for Negri bodies is still a useful method for rapid diagnosis of rabies.
- MOUSE INOCULATION TEST : Intracerebral mouse inoculation is still one of the most useful tests in the laboratory diagnosis of rabies.
- CORNEAL TEST : Rabies virus antigen can be detected in live animals in corneal impressions or in frozen sections of skin biopsies by the FRA test.
 Users Today : 1
Users Today : 1 Users Yesterday : 2
Users Yesterday : 2 Users Last 7 days : 16
Users Last 7 days : 16 Users Last 30 days : 102
Users Last 30 days : 102 Users This Month : 75
Users This Month : 75